The Ancestral Diet Is a Fairy Tale
My Alaskan Cousins
What the Inuit Story Actually Tells Us About Health
Here you have the ancestral-diet crowd, selling the modern version of a fairy tale.
They start by ignoring biochemistry. Then they wave a hand and tell you ancient man ate meat and fat and didn’t have heart disease. Apparently, when early humans stopped hunting with spears and forged them into plows, they simultaneously gained—by magic—the ability to make ApoB particles atherogenic.
And just as magically, they insist that if you adopt “ancient man’s lifestyle,” you will lose that ability again. No ApoB. No atherosclerosis. No endothelial dysfunction. Just fire pits and eternal arteries.
This isn’t science. It’s cosplay.
They invoke “ancient man” because they can make him up. He doesn’t argue back.
They cherry-pick a past where humans were apex carnivores, ignoring the fossil and archaeological evidence that early Homo sapiens were largely opportunistic—hoping for scraps from real carnivores, scavenging marrow, eating tubers, legumes, berries, shellfish, insects, and fish. Hunter-gatherer does not mean meat-only. It means whatever kept you alive.
Let’s start with what we actually have.
Today, we have enough fossilized remains of ancient Homo sapiens to fill about two school buses. We also have hundreds of thousands of living humans whose diets, outcomes, and diseases have been carefully tracked. And we have laboratory science showing—step by step—how vascular disease forms.
Atherosclerosis is not a moral failing. It is a biological process.
An ApoB-containing particle enters the bloodstream. The endothelial cell brings it in. If there are too many particles, the cell shuttles the excess out the back door—into the narrow space between the endothelium and smooth muscle. There, the particles oxidize. Macrophages arrive. Foam cells accumulate. Plaque forms.
None of this requires agriculture.
None of this requires sugar.
None of this requires seed oils.
It requires enough ApoB particles over enough time.
Case Study One: My Cousins, the Inuit
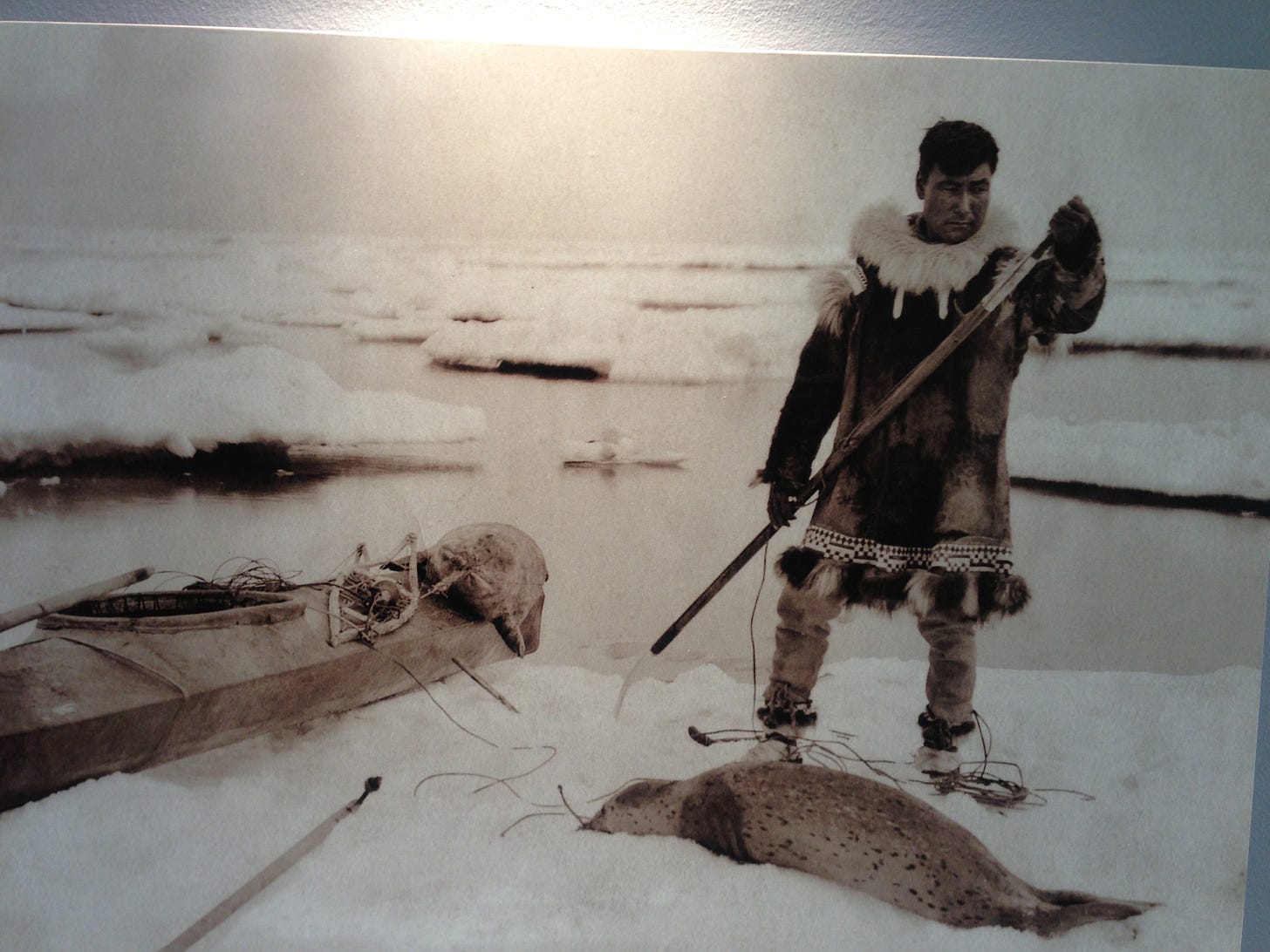
Let me start with the group most often used as proof of the ancestral-diet myth: the Inuit.
I know Inuit health not because they are my cousins—though they are—but because I was born and raised in Alaska, I am one-quarter Athabascan (yes, white as Casper the ghost—Mendelian genetics happens), and I sit on healthcare boards and committees tasked with reviewing and protecting research involving Alaska Native peoples.
Those committees exist for a reason: to prevent exploitation by outsiders more interested in owning DNA than listening to stories.
There has never been a single “Inuit diet.” Historically, diets varied by region and season—marine mammals, fish, caribou, birds, eggs, berries when available—eaten fresh, frozen, dried, or fermented. Today, some people eat largely traditional subsistence foods, some eat mostly market foods, most eat a mix.
Another myth: they lived without vitamin C.
False. Marine mammals synthesize their own vitamin C. When eaten fresh or raw—skin, organs, connective tissue—vitamin C intake was adequate. No magic ketosis. Just biochemistry.
To be clear: some carnivores think they can eat meat and get enough vitamin C and to be clear - you cannot. James Blunt, the famous singer, had a severe case of scurvy from such a diet - guess that wasn’t so beautiful.
Yes, there are genetic adaptations related to fat metabolism. Adaptations are not endorsements. They come with tradeoffs.
And no, Inuit were not free of heart disease. We have CT evidence of atherosclerosis in ancient Inuit mummified remains. Vascular disease did not arrive with supermarkets.
Today, Inuit populations continue to have high rates of colon cancer and stomach cancer, exactly as modern models predict. Vascular disease and heart disease are common, not rare. We screen. We intervene early. We track outcomes.
I would love to say that my cousins who live subsistence lives routinely live to 100 without disease. They don’t.
They are extraordinary people—but not because of a macronutrient ratio.
They are strong, proud communities with deep traditions, fierce family ties, and a remarkable capacity to rise above generations of trauma. If you want neighbors who watch out for you, move to one of these villages.
Strength Forward: What We Led
Alaska Native communities do not define themselves by deficiency. We define ourselves by response.
Some of the earliest smallpox vaccinations in the New World occurred among the Aleut through variolation. When tuberculosis ravaged communities, Alaska helped lead early streptomycin trials that proved TB could be treated.
When COVID vaccines became available, Alaska Native health systems moved fast. Hospital employees were mandated to be vaccinated—by unanimous decisions of elder-led boards—because history taught us that hospitals must never become places where a worker’s breath infects an auntie or uncle.
When hepatitis B devastated children with liver failure, we partnered with public health experts and implemented infant vaccination. We now have forty years of real-world proof that it works.
This is what strength looks like.
A hard truth about children and keto
One final warning.
Among some Alaska Native children, there is a well-described variant involving carnitine palmitoyltransferase 1A (CPT1A)—an enzyme essential for fat metabolism during fasting and illness.
When these children enter ketosis, they cannot generate energy safely. The result can be hypoglycemia, metabolic crisis, and sudden infant death.
Keto is not “natural” for everyone.
For some children, it is dangerous.
And ancestral mythology does not protect them.
A Necessary Pause: Whole Food Is Good — But It Isn’t Magic
Before we go any further, let’s be clear about something that often gets lost in these arguments.
Whole food is good.
We like whole food.
You often hear the advice: shop the outside of the grocery store. Buy fresh produce, real food, things your grandmother would recognize. That’s not bad advice—if you can do it.
But imagine telling my cousins on St. Paul Island to “just buy fresh produce.”
Do you have any idea how hard it is to get fresh vegetables there?
Now imagine saying the same thing to someone living in a food desert on the South Side of Chicago. Advice that ignores access isn’t wisdom—it’s privilege dressed up as nutrition.
Yes, eating great food matters.
Yes, whole food matters.
Yes, plant-forward eating matters.
In short: the Mediterranean diet is a great idea.
I eat that way. I recommend it. I teach it.
But here’s where another fairy tale sneaks in.
As much as I would love for a perfect diet to free me from medications—
whether it’s the GLP-1 I take for obesity
or cholesterol-lowering medication for the familial hypercholesterolemia I carry—
…it doesn’t work that way.
I eat Mediterranean.
I am not perfect.
And I will take medication for my chronic diseases until my last breath—hopefully a long time from now.
That isn’t failure.
That’s adulthood.
If your version of “ancestral eating” has turned into a purity test—where you won’t eat broccoli because it somehow violates a prehistoric fantasy—then I might gently suggest you haven’t grown up yet.
Eat your vegetables.
And don’t imagine that hunter-gatherer diets were remarkable for anything other than this:
they kept people alive long enough to reproduce.
They were not optimized for longevity.
They were not optimized for freedom from disease.
They were optimized for survival.
Most of my family in Alaska also has high cholesterol and needs medication. Ancestry didn’t repeal biology.
And let me add one final reality check:
I doubt most of you would enjoy the taste of seal or walrus.
I do, however, love salmon—and eat it often.
So yes:
Eat whole food when you can
Eat plant-forward when possible
Use diet to support health
But don’t turn food into a religion.
And don’t confuse nutrition with absolution.
Diet can help.
It cannot erase human biology.
🔒 What’s in the Paid Section
In the subscriber section, we slow this down and look at what the data actually show, not what diet ideology promises.
You’ll get:
What ancient imaging and modern registries really tell us about Inuit heart disease—then and now
Why colon and stomach cancer rates remain high and what actually changes outcomes
A clear explanation of ApoB biology and why atherosclerosis doesn’t disappear with latitude or macronutrient ratios
The CPT1A mutation and why ketogenic diets can be dangerous for some children
How infectious disease exposure—not genetics— devastated Indigenous communities
Why healthcare systems, screening, and trust matter more than ancestral mythology
If you want folklore, the internet has plenty.
If you want mechanisms, outcomes, and uncomfortable truths—subscribe
.