Why are younger people getting colon cancer?
The rise is real, the reason is ....
The Rise of Colon Cancer in Younger Adults
There has been a rise in colon cancer among younger people, and when someone like James Van Der Beek (died age 44) of Dawson’s Creek or Chadwick Boseman of Black Panther (who died at 43) is diagnosed, people ask the same question:
Why?
We used to think of colon cancer as a disease of retirement. A disease that appeared after decades of life. A disease of the 60s and 70s.
That assumption is no longer safe.
Early-onset colorectal cancer — defined as diagnosis before age 50 — now accounts for roughly 14% of all colorectal cancers, up from about 10–11% just a decade ago. In 1995, about 1 in 10 colorectal cancers occurred in adults 54 or younger. By 2019, it was 1 in 5.
Among adults under 40, incidence has risen steadily. Among 20–29 year olds, rectal cancer rates have climbed by roughly 3–4% per year. Those born around 1990 face roughly double the risk of colon cancer — and up to four times the risk of rectal cancer — compared to those born around 1950.
This is not better detection alone.
This is a birth-cohort effect.
Something changed.
What Changed?
When disease patterns shift across generations, we look for environmental shifts interacting with biology.
The human genome does not mutate that fast.
The environment does.
Genetics — Important, But Insufficient
Yes, hereditary syndromes matter. Roughly 16–25% of early-onset cases involve identifiable germline mutations such as Lynch syndrome.
But that means most cases do not.
If this were purely genetic, we would not see this kind of generational acceleration.
Genetics loads the gun. Environment pulls the trigger.
The Metabolic Generation
Obesity nearly doubles the risk of early-onset colorectal cancer.
Childhood and adolescent obesity increases lifetime risk. Maternal obesity appears to influence risk in offspring.
We are now watching the first fully “metabolic generation” — raised in an environment of ultra-available calories, high glycemic load, sedentary entertainment, and disrupted sleep — enter their 30s and 40s.
Colon cancer is not sudden. It is the endpoint of years of inflammatory signaling.
Hyperinsulinemia.
Elevated IGF-1 pathways.
Chronic low-grade inflammation.
Altered immune surveillance.
The soil changes long before the tumor appears.
Ultra-Processed Foods and the Microbiome
Ultra-processed foods now account for nearly 60% of caloric intake in American adults.
These foods tend to be:
Low in fiber
Low in micronutrients
Low in phytochemicals
High in refined starch
High in emulsifiers and additives
Emerging research links higher ultra-processed food intake to increased risk of precancerous adenomas and early-onset colorectal cancer.
This is not about one ingredient.
It is about dietary pattern.
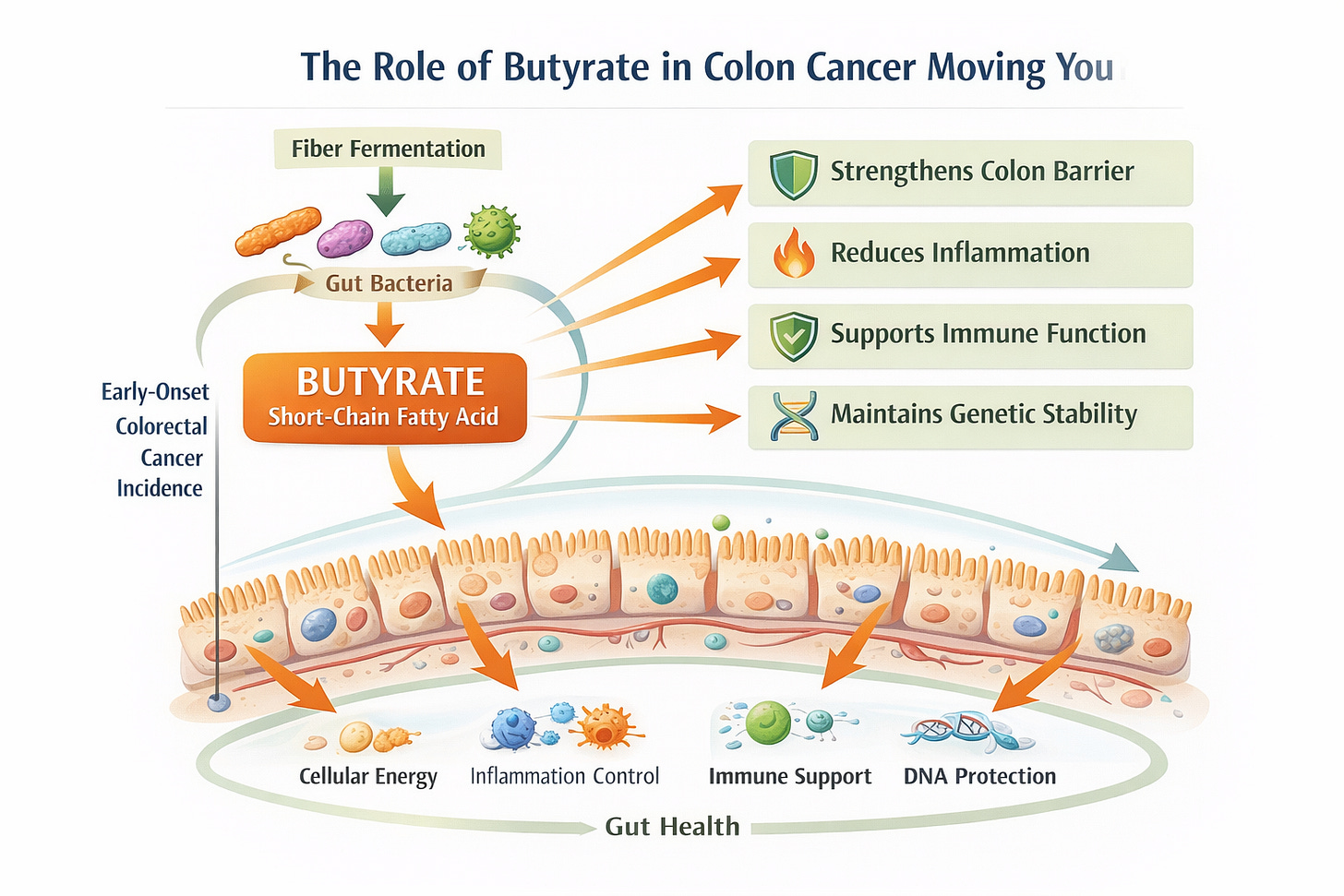
Fiber intake has declined in many populations. Fiber feeds butyrate-producing bacteria in the colon. Butyrate supports mucosal integrity and regulates inflammation.
When fiber drops, the microbiome shifts.
Certain organisms — Fusobacterium nucleatum, toxin-producing strains of E. coli, and others — have been identified more frequently in early-onset colorectal cancer. Some of these bacteria produce genotoxins. Others promote immune evasion.
The colon is not just a tube.
It is an ecosystem.
And ecosystems respond to diet.
Sugar-Sweetened Beverages and Adolescent Exposure
Two or more sugar-sweetened beverages per day during adolescence more than doubles the risk of early-onset colorectal cancer, compared with less than one per week.
Each additional daily serving in teenage years increases risk substantially.
That matters.
We are watching the first generation raised on ubiquitous soda and sweetened beverages, like the coffees, reach midlife.
Teenage exposures appear to leave a metabolic imprint.
Sedentary Life
Physical inactivity is not neutral or even natural.
Sedentary behavior — particularly high screen time — has been associated with increased colon cancer risk. Physical activity reduces risk by roughly 30%.
Movement alters insulin sensitivity, inflammation, and immune function.
The modern environment makes inactivity easy.
Biology was not built for that.
Antibiotics and Early-Life Microbiome Disruption
Long-term or repeated broad-spectrum antibiotic exposure in early life has been associated with increased early-onset colorectal cancer risk years later.
The data are mixed — but the mechanism is plausible.
Antibiotics reshape the microbiome.
The microbiome influences immune regulation.
Immune regulation influences cancer surveillance.
We are only beginning to understand the downstream consequences of early-life microbial disruption.
This is another reason when your doctor says that you don’t need an antibiotic, please believe them.
The Hardest Part
Some of the most tragic cases I have treated were in people who:
Exercised regularly
Were lean
Ate reasonably
Had no known hereditary syndrome
Colon cancer does not check your gym membership.
Looking healthy is not a guarantee.
Colorectal cancer remains one of the leading causes of cancer death in the United States. Among adults aged 20–49, it has become one of the top causes of cancer-related mortality.
That is not a statistic we should be comfortable with.
Screening Is Not Optional

Lifestyle modification is important.
But it does not erase accumulated risk.
Colonoscopy does not just detect cancer.
It prevents it by removing polyps before they become malignant.
If you are 45, screen.
If you have symptoms — rectal bleeding, iron deficiency anemia, change in bowel habits, unexplained weight loss — do not wait.
Screening is for people who feel well.
Evaluation is for people with symptoms.
The two are not the same.